Hedis Training Course
Hedis Training Course - Through hedis, ncqa compares aetna better health ® of illinois. Hedis is a nationally standardized set of measures. It’s a challenging time for keeping teams. Currently consisting of 94 measures across seven domains of care, hedis is maintained by the. The next exam review and session will be held on september 17 & 18, 2025. To become a certified hedis ® compliance auditor, you must pass the hedis compliance audit™ exam. Best practices for improving hedis results. Explore our premier hedis training course, a thorough curriculum created to provide learners with a thorough grasp of quality improvement techniques, data gathering, and hedis metrics. Hedis compliance audits review whether organizations have capabilities for processing medical, member and provider information as a foundation for accurate and automated performance. Hedis is a set of standardized performance measures developed by the national committee for quality assurance (ncqa). Hedis course equips you with the knowledge and skills needed to navigate quality reporting requirements, analyze healthcare data effectively, and contribute to initiatives aimed at. Best practices for improving hedis results. Hedis is a set of standardized performance measures developed by the national committee for quality assurance (ncqa). Blue cross and blue shield of illinois (bcbsil) reports audited healthcare effectiveness data and information set (hedis) results. Virtual training for your team from ncqa experts on hedis ®, accreditation and more. Currently we provide hedis abstraction training courses. The next exam review and session will be held on september 17 & 18, 2025. It’s a challenging time for keeping teams. As the developer of hedis ®, ncqa offers training on: Currently consisting of 94 measures across seven domains of care, hedis is maintained by the. Currently consisting of 94 measures across seven domains of care, hedis is maintained by the. This training presented by ncqa staff gives you an inside look at to the latest developments in hedis and designed to help participants stay ahead of the curve with the most current. Blue cross and blue shield of illinois (bcbsil) reports audited healthcare effectiveness data. Hedis compliance audits review whether organizations have capabilities for processing medical, member and provider information as a foundation for accurate and automated performance. Best practices for improving hedis results. Currently consisting of 94 measures across seven domains of care, hedis is maintained by the. It’s a challenging time for keeping teams. Hedis is a nationally standardized set of measures. Currently consisting of 94 measures across seven domains of care, hedis is maintained by the. Hedis is a set of standardized performance measures developed by the national committee for quality assurance (ncqa). This training presented by ncqa staff gives you an inside look at to the latest developments in hedis and designed to help participants stay ahead of the curve. Hedis course equips you with the knowledge and skills needed to navigate quality reporting requirements, analyze healthcare data effectively, and contribute to initiatives aimed at. Blue cross and blue shield of illinois (bcbsil) reports audited healthcare effectiveness data and information set (hedis) results. The next exam review and session will be held on september 17 & 18, 2025. It’s a. As the developer of hedis ®, ncqa offers training on: Currently consisting of 94 measures across seven domains of care, hedis is maintained by the. Hedis course equips you with the knowledge and skills needed to navigate quality reporting requirements, analyze healthcare data effectively, and contribute to initiatives aimed at. Through hedis, ncqa compares aetna better health ® of illinois.. As the developer of hedis ®, ncqa offers training on: This training presented by ncqa staff gives you an inside look at to the latest developments in hedis and designed to help participants stay ahead of the curve with the most current. Hedis compliance audits review whether organizations have capabilities for processing medical, member and provider information as a foundation. Virtual training for your team from ncqa experts on hedis ®, accreditation and more. This training presented by ncqa staff gives you an inside look at to the latest developments in hedis and designed to help participants stay ahead of the curve with the most current. As the developer of hedis ®, ncqa offers training on: Hedis is a nationally. Best practices for improving hedis results. Hedis is a set of standardized performance measures developed by the national committee for quality assurance (ncqa). This training presented by ncqa staff gives you an inside look at to the latest developments in hedis and designed to help participants stay ahead of the curve with the most current. Explore our premier hedis training. Hedis is a set of standardized performance measures developed by the national committee for quality assurance (ncqa). It’s a challenging time for keeping teams. Best practices for improving hedis results. Hedis compliance audits review whether organizations have capabilities for processing medical, member and provider information as a foundation for accurate and automated performance. Hedis course equips you with the knowledge. As the developer of hedis ®, ncqa offers training on: To become a certified hedis ® compliance auditor, you must pass the hedis compliance audit™ exam. Currently we provide hedis abstraction training courses. Through hedis, ncqa compares aetna better health ® of illinois. Hedis is a set of standardized performance measures developed by the national committee for quality assurance (ncqa). Blue cross and blue shield of illinois (bcbsil) reports audited healthcare effectiveness data and information set (hedis) results. It’s a challenging time for keeping teams. Hedis course equips you with the knowledge and skills needed to navigate quality reporting requirements, analyze healthcare data effectively, and contribute to initiatives aimed at. Currently consisting of 94 measures across seven domains of care, hedis is maintained by the. To become a certified hedis ® compliance auditor, you must pass the hedis compliance audit™ exam. Best practices for improving hedis results. Hedis is a nationally standardized set of measures. The next exam review and session will be held on september 17 & 18, 2025. As the developer of hedis ®, ncqa offers training on: Ignite and empower your team with ncqa’s group training. Explore our premier hedis training course, a thorough curriculum created to provide learners with a thorough grasp of quality improvement techniques, data gathering, and hedis metrics. Currently we provide hedis abstraction training courses. Hedis compliance audits review whether organizations have capabilities for processing medical, member and provider information as a foundation for accurate and automated performance.HEDIS Course for Seasonal Remote Nursing Jobs Remote Nurse Connection
Vital Data Technology Earns NCQA Certification for HEDIS® Measurement
Afia is NCQA Certified on 13 HEDIS Measures Afia
Expert HEDIS Training Courses HEDIS Abstraction & More
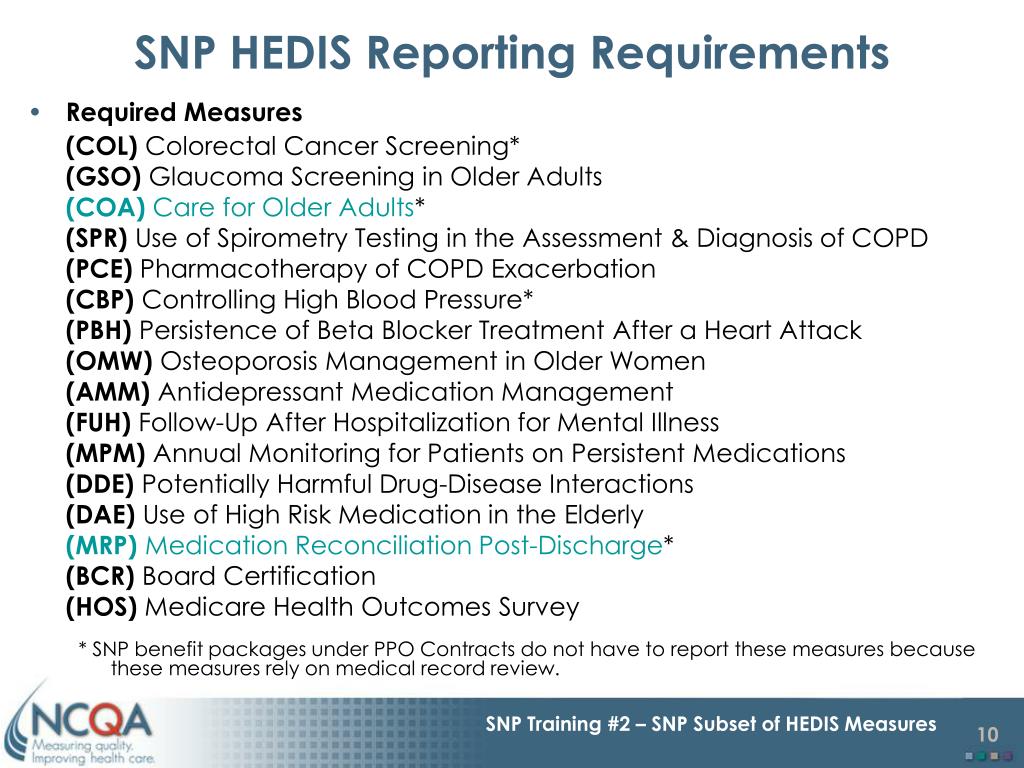
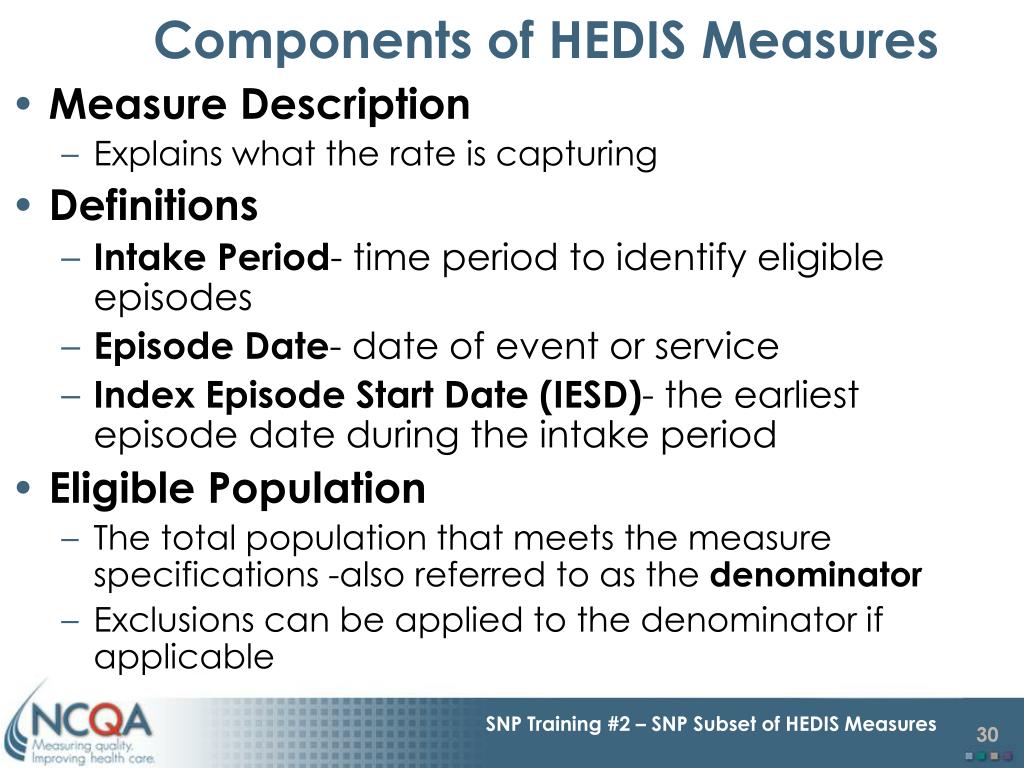
PPT SNP Training Topic 2 SNP Subset of HEDIS Measures PowerPoint
HEDIS Course for Seasonal Remote Nursing Jobs Remote Nurse Connection
Cotiviti achieves 20 years of HEDIS® certification amid expanding
HEDIS Course for Seasonal Remote Nursing Jobs Remote Nurse Connection
PPT SNP Training Topic 2 SNP Subset of HEDIS Measures PowerPoint
HEDIS Course Remote Nurse Connection
Through Hedis, Ncqa Compares Aetna Better Health ® Of Illinois.
Hedis Is A Set Of Standardized Performance Measures Developed By The National Committee For Quality Assurance (Ncqa).
This Training Presented By Ncqa Staff Gives You An Inside Look At To The Latest Developments In Hedis And Designed To Help Participants Stay Ahead Of The Curve With The Most Current.
Virtual Training For Your Team From Ncqa Experts On Hedis ®, Accreditation And More.
Related Post:
.png?width=1106&name=HEDIS Interim Cert. 2022 (5).png)